Technologies
Viz.aiDemocratizing Diagnosis and Treatment:
An Interview with Chris Mansi of Viz.ai
What is the need you set out to address?
Chris: I was very aware from my work as a neurosurgeon, and from my time with Biodesign, that developing a new device or drug to treat a patient wasn't enough. Challenges with workflow in healthcare would likely mean that not all patients benefit from available treatments. There had to be a better way to make healthcare work faster and smarter.
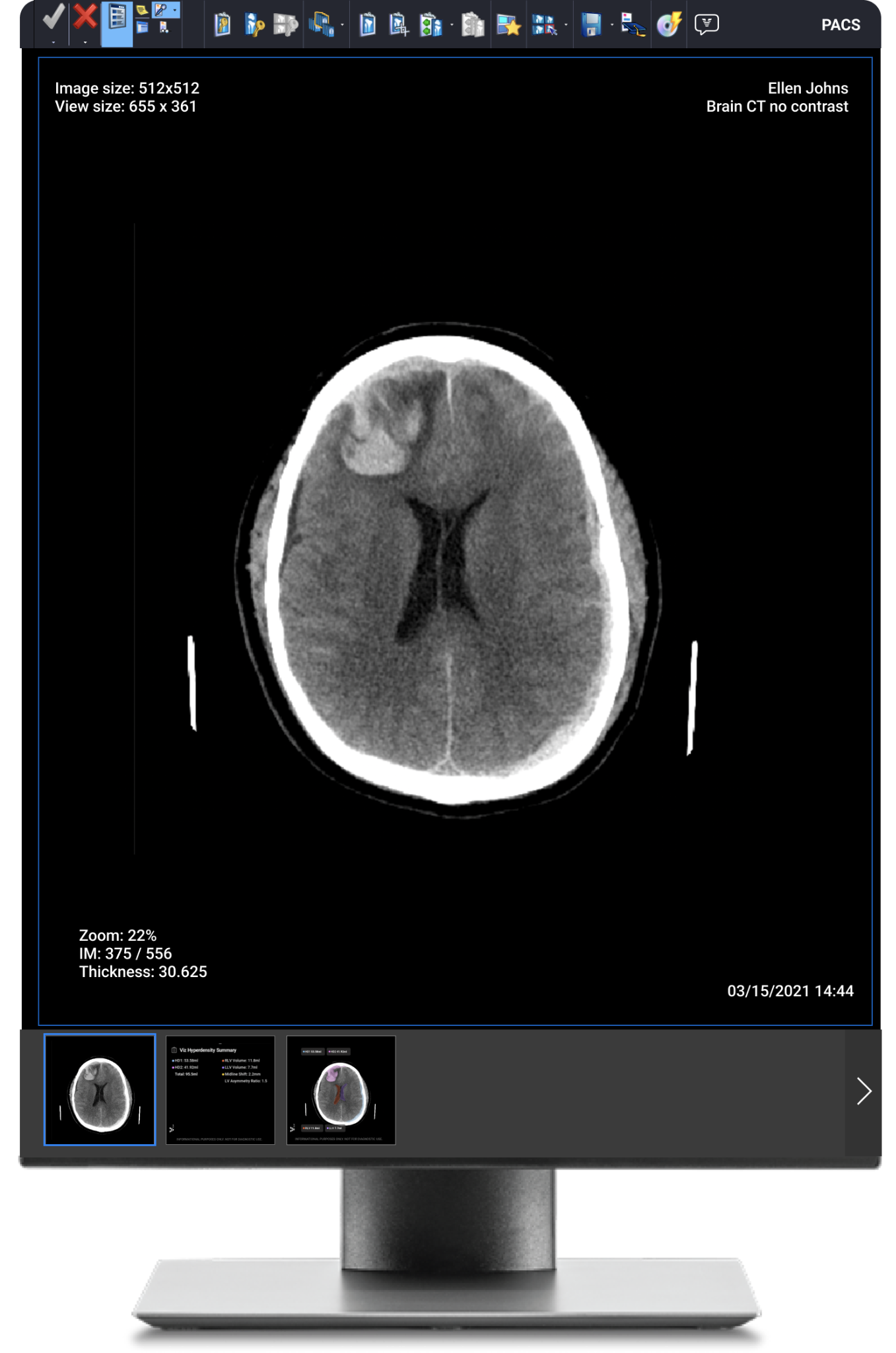
We started in ischemic stroke, where time really matters. Our initial focus was on thrombectomy, which is a very effective treatment for a large vessel occlusion stroke. But only about two percent of patients actually get the treatment, and the reason came down to luck. If the patient was taken to a comprehensive stroke center like Stanford, a radiologist, a neurologist, and a neurosurgeon would all be on-hand to coordinate care and get the patient into treatment. But if the patient was at a different hospital, they would have to depend on an emergency room physician, who rarely sees a large vessel occlusion stroke and may not be familiar with thrombectomy treatment. So, the chances of being quickly transferred and effectively treated were really low. Back when Viz.ai were starting out, the median time to treatment for stroke patients was three hours for a comprehensive center, but five hours for other facilities without a specialist treating physician.
In the stroke world, we say ‘time is brain’ because every minute two million patient brain cells die. Stroke is the number one cause of long-term disability in the United States. So, bringing the time to treatment down from five hours to under an hour delivers huge benefits to patients and their families, and it substantially reduces the burden on the health system and payers.
What key insight was most important to guiding the design of your solution?
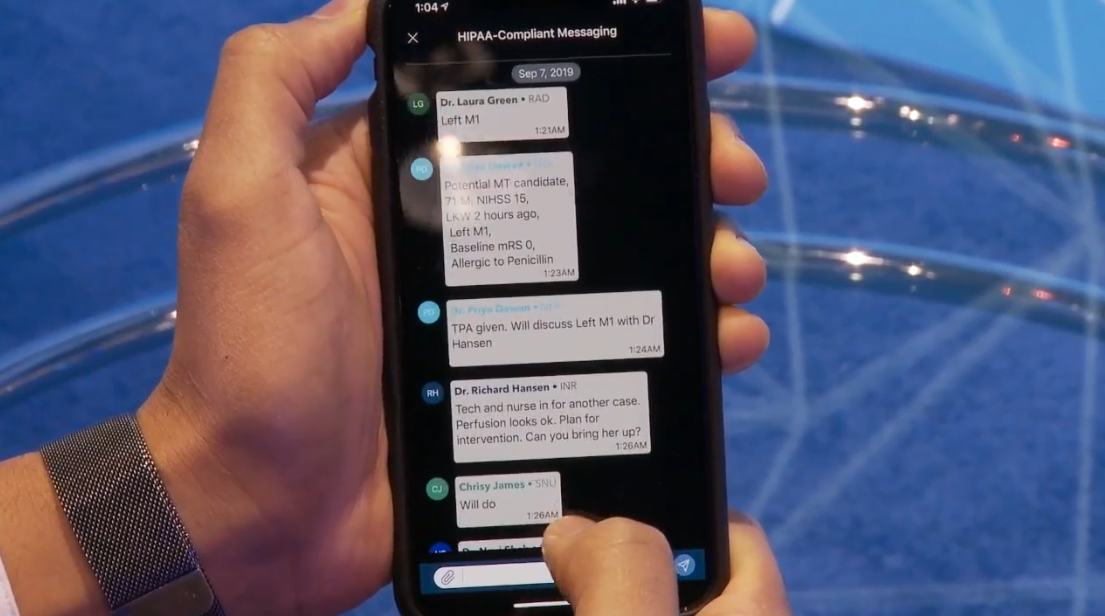
We knew that an AI-based technology could interpret a scan, but we realized that to actually make it clinically useful, we needed the interpretation to drive workflow. So, our focus wasn't about helping radiologists be better at their jobs, it was about coordinating care between the emergency room, radiology, neurology, and neurosurgery. And that insight has translated into everything we do, whether it's a condition where minutes matter, like stroke, or taking diagnosis from 5 years down to five days, like hypertrophic cardiomyopathy. I believe that the medical innovation field will find ways to cure almost every disease through the amazing work happening in biotechnology and medical devices, but the problem is that so few patients are going to benefit from that unless we have a system that directly connects the patient who needs the treatment with the person who can diagnose and prescribe or perform the treatment.
 Viz.ai co-founders Chris Mansi and David Golan.
Viz.ai co-founders Chris Mansi and David Golan.
Another big insight was centered on democratizing care. We realized that AI-driven technology, that worked in the same manner every time could help by reducing the bias that we have in human healthcare. This bias might be based on which hospital the patient attends, what time of day or night it is, how tired the doctor is, and what cases the particular doctor is familiar with. From our very first FDA study in stroke, we were targeting a reduction in time-to-treatment, and we accomplished that by showing an hour-long time decrease with the software. But if you look at the study results, we also reduced the standard deviation in time-to-treatment by two hours. We took it from 127 minutes down to seven minutes. That’s what our technology can do very well – reduce variability of care. It works the same at any time of day and whether the patient is at Stanford or in rural Mississippi. And it's not reliant on the clinical literature that each doctor has read or the conferences they've recently attended. Hence, we’re able to truly democratize care.
"That’s what our technology can do very well – reduce variability of care. It works the same at any time of day and whether the patient is at Stanford or in rural Mississippi."
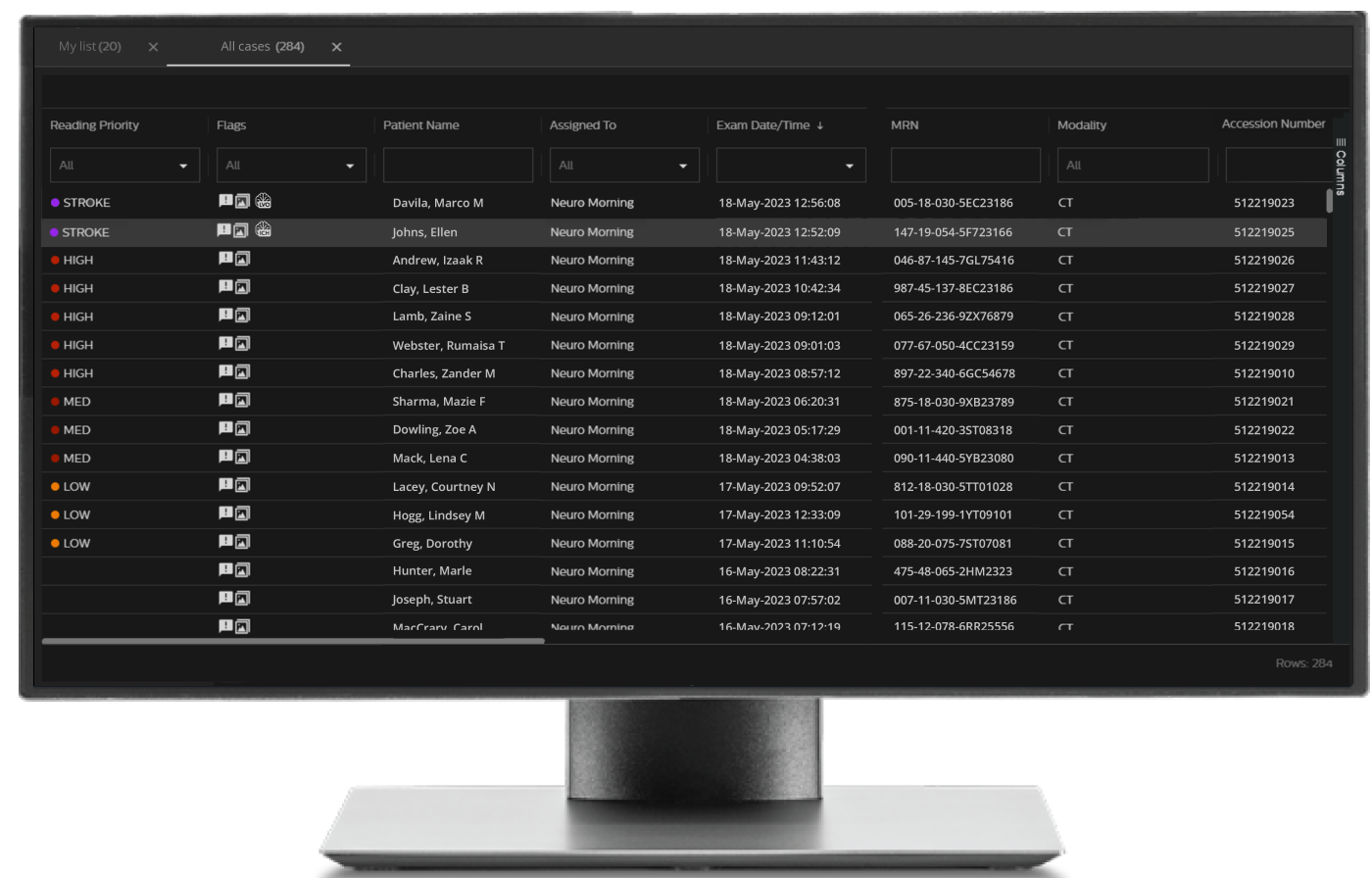
How does your solution work?
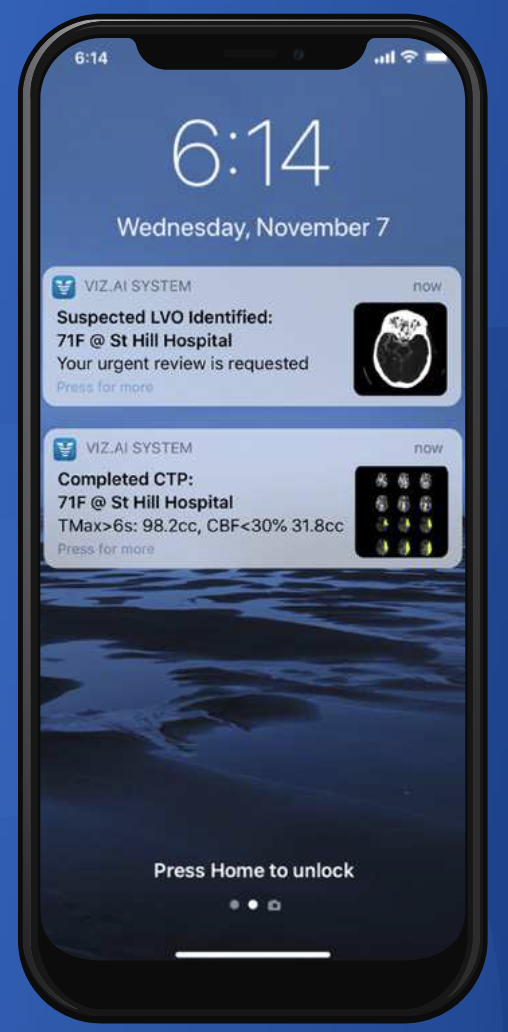
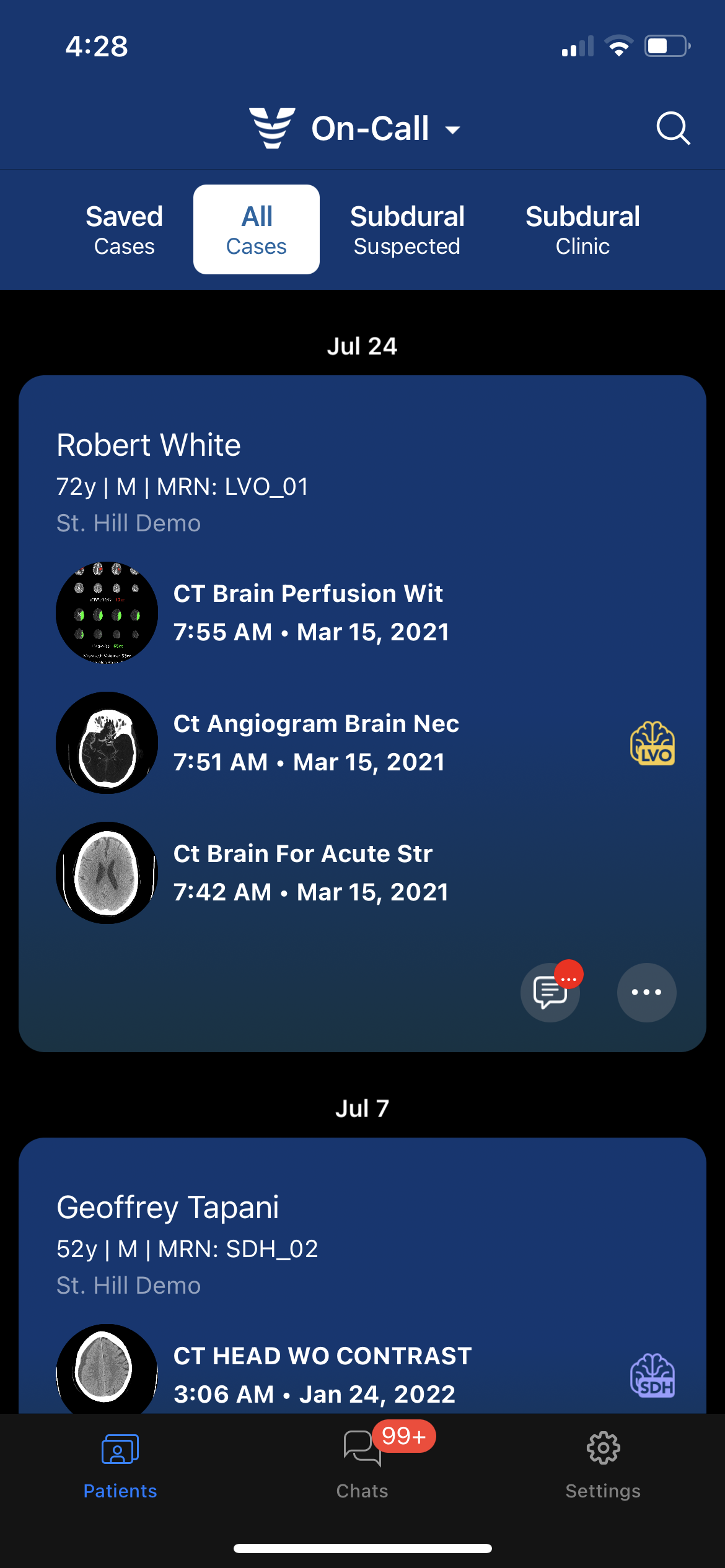
We like to contrast our technology with an electronic health record. The electronic health record is the system of record in a hospital, storing an exponentially increasing amount of medical data and enabling note taking, billing, etc. In contrast, Viz.ai is a system of action. It transforms workflows by facilitating the fast and accurate detection of diseases, using an AI read of imaging and other patient data, and automatically sharing relevant scans and other information to enable quicker transfers and better collaboration between the care teams at treating and referral hospitals to accelerate time-to-treatment.
 The Viz.ai platform is intended to improve the accuracy and speed of diagnosis and treatment (see endorsement disclaimer below).
The Viz.ai platform is intended to improve the accuracy and speed of diagnosis and treatment (see endorsement disclaimer below).
At what stage of development is the solution?
The commercial launch of the first stroke product was in 2018, the first of its kind to be approved by the FDA. Viz.ai now has FDA-cleared software that addresses 12 disease areas, with many more in the pipeline across the neurology, cardiology, and vascular domains. Oncology is the next area we're entering.
Currently, 1,500 sites use the technology, with the majority in the US. We also are collaborating with seven of the top 30 life science companies, such as Bristol Myers Squibb and Medtronic, on the development and deployment of AI-powered workflows. One of the metrics we track is how often patients are helped by our software. Right now, we help a patient every 13 seconds.
Tell us about a major obstacle you encountered and how you overcame it.
We were the first-ever AI software system to get a new technology add-on payment [NTAP] from CMS in 2020. When we received it, the world of AI was astounded as they thought it was 10 years away. When we first started the CMS process, experts in the field told us we had ‘a snowball’s chance in hell’ of getting it because it has been very hard to quickly generate enough data to show that you’re making a substantial clinical improvement.
"When we first started the CMS process, experts in the field told us we had ‘a snowball’s chance in hell’ ...."
We worked with medical societies, hospitals, and providers to quickly produce data on how well the Viz software was working in the real-world setting. We had to rally all of the stroke world – the AHA, the Society of Vascular and Interventional Neurology, the Society of Neurointerventional Surgery, numerous key opinion leaders, and many of the hospitals we were working with – to present data to CMS and write letters of support on why this mattered to the populations they cared for. We got Congress members involved. We engaged advisory firms. It was a big lift and a huge team effort. It took about 18 months and several million dollars to make it happen. But we ended up being awarded reimbursement of $1,040 every time the software is used, which is a great outcome for hospitals, patients, and payers. And we were proud to have achieved it against the odds.
What role did your Biodesign training play in enabling you to design, develop, and/or implement this solution?
Viz.ai wouldn't be here without Stanford Biodesign. Biodesign was fundamental for understanding clinical needs finding and financial needs finding. To be successful in launching a healthcare business, you have to have that dual value prop.
Also, you can’t be a know-it-all physician and take an ivory tower approach and assume you understand everything that’s going on for the patient. You have to go spend time in a real world clinical setting and find out what is really happening, and where things are breaking down. I spent many, many weeks traveling around in a car through North Carolina, Tennessee, and Georgia to really understand the status quo. It became obvious that, while the workflow was reasonably well optimized at most comprehensive stroke centers, the stroke specialists had little insight into what was happening at the hospitals referring patients to them. They would simply get a call about a patient, and they would work quickly to get the patient transferred to their hospital, but they weren't aware that maybe 1 in 10-100 eligible patients were actually reaching them. Biodesign’s approach of taking a step back and doing a root cause analysis of the clinical need area at the systems level really led to the insights that made Viz.ai successful.
What advice do you have for other innovators about health technology innovation?
You have to get the fundamentals of helping the patients right AND you also have to understand the flow of money and the interests of the other relevant stakeholders. No matter what the disease area is, it’s essential to understand the entire ecosystem.
Another piece of advice is related to regulation and reimbursement. Hire people who really understand the rules of the game in those areas. The people in FDA and CMS can help you bring innovative technologies to market, but you have to translate things for them. Be humble and understand how they think about the world because it’s different from the Stanford or Silicon Valley way of thinking.
Chris Mansi co-founded Viz.ai in 2016 after taking the graduate-level Biodesign Innovation course during his time at Stanford.
Disclaimer of Endorsement: All references to specific products, companies, or services, including links to external sites, are for educational purposes only and do not constitute or imply an endorsement by the Byers Center for Biodesign or Stanford University.