Technologies
Vynca Health Honoring Patient Wishes at the End of Life –
An Interview with Rush Bartlett and Ryan Van Wert of Vynca Health
What is the need you set out to address?
Rush: When we were Biodesign Innovation fellows, we met for coffee with Dr. Allen Namath, who was a critical care physician at Stanford. As we were talking, I asked him, ‘What’s the worst part of your job?’ In response, he told us the story of a 90 year-old woman who he recently helped resuscitate. In doing so, he inadvertently broke some of her ribs. The next day, her daughter arrived from out of town and discovered her mother on life support. Only then did he learn that the woman had a ‘do not resuscitate’ order in place. Ultimately, Dr. Namath had to withdraw care, which took time since the woman had to be ethically weaned off her medication and sedation. The whole experience took a physical toll on the patient, caused emotional distress for the family and the medical team, and resulted in costly unwanted care.
“The problem was that accurate information about patient’s end-of-life wishes was not readily and consistently available in the electronic health record….”
As we dug into the problem, we learned that this happened relatively frequently – at least once a week just at Stanford Hospital. The problem was that accurate information about patient’s end-of-life wishes was not readily and consistently available in the electronic health record [EHR] in those few critical moments when decisions are made about putting somebody on life support or not. So our need statement was ‘A way to provide rapid access to a patient's code status in the event of an emergency in order to avoid unwanted hospitalization.’
What key insight was most important to guiding the design of your solution?
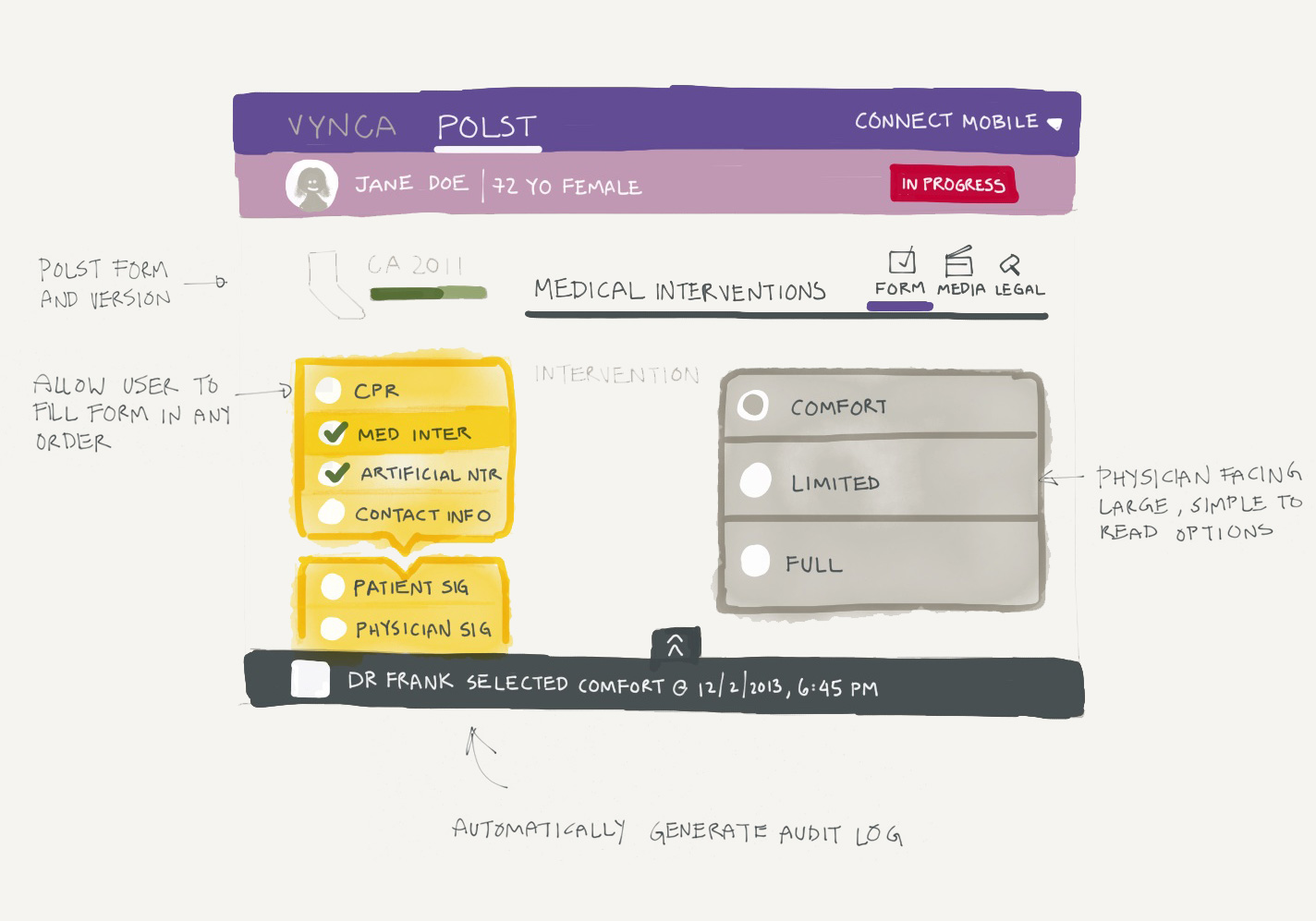
Ryan: We knew that system interoperability would be essential from the start. What we didn’t initially anticipate was how important it would be to improve the quality of the information going into the system. Discussing and documenting end-of-life choices is a challenging and complex process for the individual, their family, and the provider. There’s lots of discomfort about what to say, how to say it, and what specific choices mean. We quickly realized that part of the solution had to help guide these conversations so that important topics are addressed and patient wishes are captured in a way that is uniformly clear to providers and caregivers.
 Co-founders Rush Bartlett and Ryan Van Wert.
Co-founders Rush Bartlett and Ryan Van Wert.
How does your solution work?
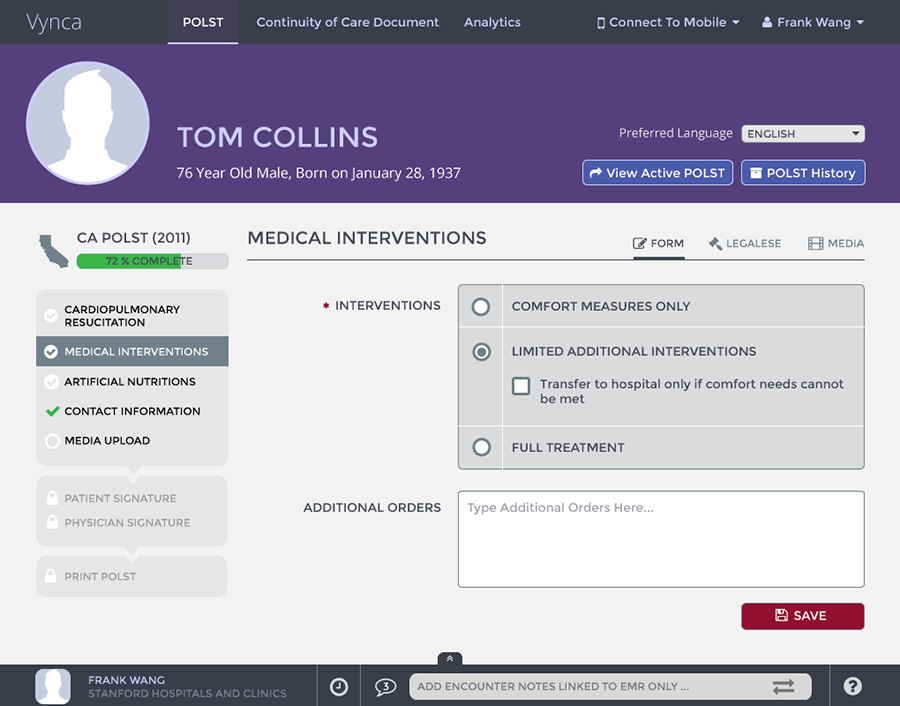
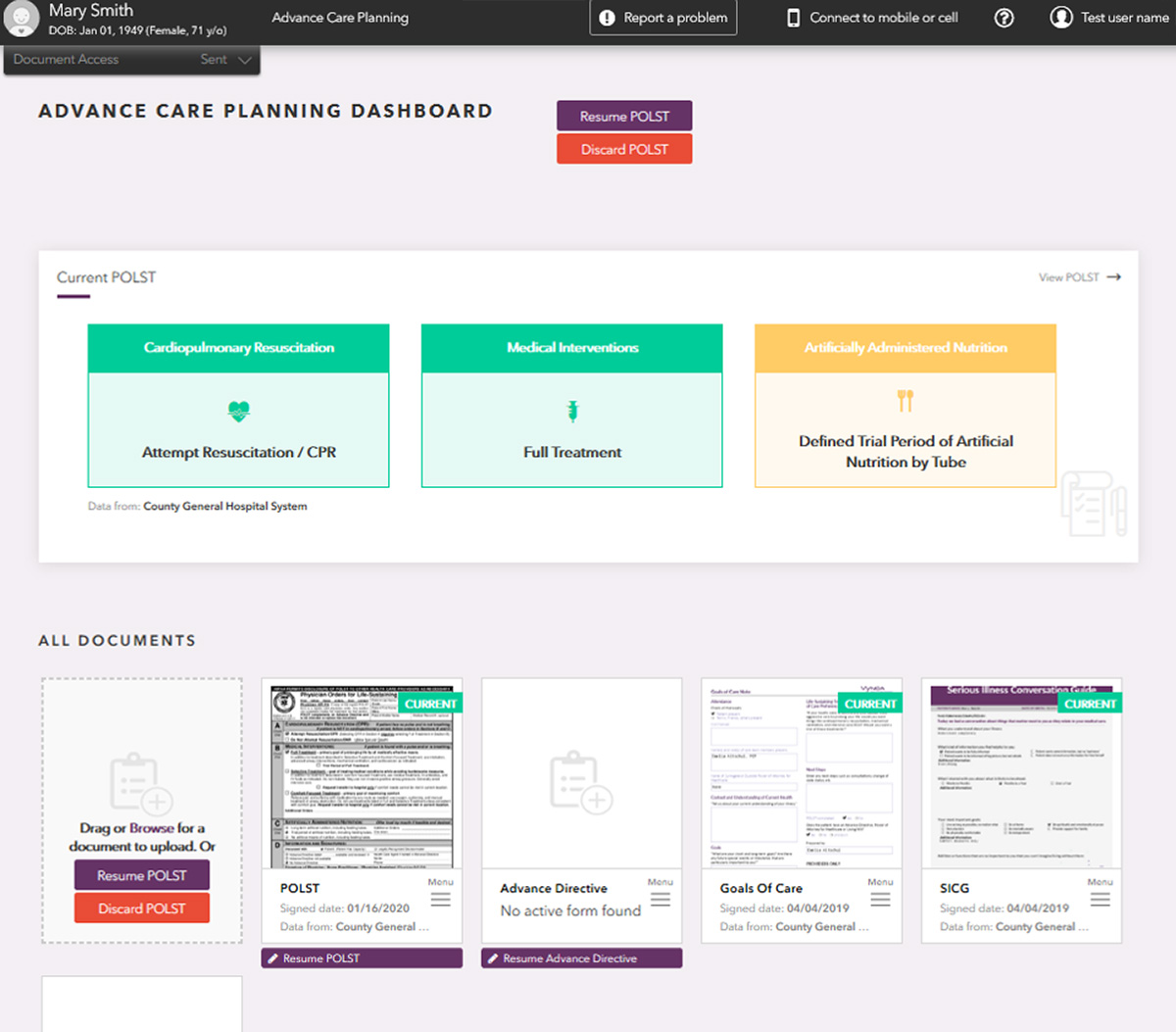
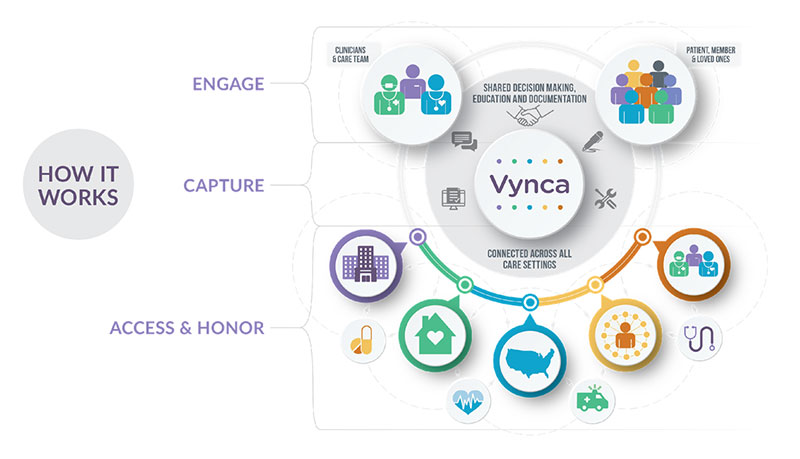
Ryan: Vynca offers a complete, end-to-end, EHR-integrated advance care planning solution. From shared decision making to the electronic completion of advance care planning documents – advance directives, POLST and others – we make critical information available to clinicians, patients, and their designated family members to help ensure that end-of-life wishes are honored and unwanted medical care is avoided.
Importantly, we also offer a high touch consultative service model that supports healthcare organizations in developing and implementing processes that facilitate clear and specific end-of-life discussions, as well as patient engagement tools to educate individuals on their choices and help them make informed decisions.
 Vynca offers a complete, end-to-end, EHR-integrated advance care planning solution.
Vynca offers a complete, end-to-end, EHR-integrated advance care planning solution.
At what stage of development is the solution?
Ryan: The technology is commercially available. At present, we have more than 600,000 patient care plans in the system, across 11 states. Five of those are operating what's called a state registry for universal access of the end-of-life documents. More than 100 hospitals are using Vynca, and we recently were adopted by our first health plan.
So far, organizations using the solution have realized a 37% reduction in hospital admissions, a 59% reduction in ICU utilization, and a 2x increase in completed end-of-life documents.
Tell us about a major obstacle you encountered and how you overcame it.
Rush: In our case, it was finding our first customer. We had to convince a large academic medical center that four kids from Stanford were not going to bring down their EHR system as we implemented the solution and shared millions of patient records back to ensure that patients actually got the care they wanted.
“We had to convince a large academic medical center that four kids from Stanford were not going to bring down their EHR system as we implemented the solution….”
As it turned out, we happened to connect with Oregon Health and Science University, the nation's largest and most prestigious research center on the topic of end-of-life care, right as they were trying to figure out how to electronically connect their EHR with the state end-of-life registry. They had actually prototyped a system but, as a nonprofit, they couldn’t afford the technical talent needed to make it work. So when we showed up with some of the smartest software engineers in the world and a willingness to work with them to co-develop and test the system, they were on board. And, together, we were able to overcome the technical challenges and achieve the social aim of effectively communicating patient’s end-of-life care preferences.
What role did your Biodesign training play in enabling you to design, develop, and/or implement this solution?
Rush: There are three important things I credit to the Biodesign approach. The first is finding the right unmet need. The second is developing the right solution to the unmet need, because if you just devise the quickest, easiest solution you’ll ultimately be passed by someone else who solves the problem in a way that better meets stakeholder needs. And third is finding the right talent to help you implement the right solution for the right unmet need.
What advice do you have for other innovators about health technology innovation?
Ryan: My favorite advice for innovators comes from Thomas Fogarty who said, ‘The path to successful innovation is very often lonely and frustrating. Innovation by its very definition means something different than what exists. Basically, we are defying standards and sometimes basic concepts. Be prepared to be criticized, ostracized, called crazy, inappropriate, outlandish, stupid, intolerable, and bound to fail…. Take solace from the fact that these challenges can be a useful part of the process of innovation…. Ultimately, your ability to prevail through these challenges will benefit patients, caregivers and institutions.’
Rush Bartlett and Ryan Van Wert launched Vynca Health out of the Biodesign Innovation Fellowship in 2013. More information is available online.
Disclaimer of Endorsement: All references to specific products, companies, or services, including links to external sites, are for educational purposes only and do not constitute or imply an endorsement by the Byers Center for Biodesign or Stanford University.