Technologies
Windmill Revolutionizing Neonatal Resuscitation:
An Interview with Avijit Bansal of Windmill Health
What is the need you set out to address?
Our need focused on a way to empower front-line health workers to resuscitate newborns with birth asphyxia more easily and effectively. I was motivated to tackle this need by several experiences. First, when I was pretty young, I saw my mother resuscitate a 12-year-old boy. He collapsed and was gone. But, with a few minutes of resuscitation, he came back to life. That left a powerful impact on me. The second was when I was an intern in the labor room, where I experienced firsthand the anxiety when a baby is about to be born; but what if they don't breathe? That worry can be an overwhelming emotion. Finally, as I started looking into the space, I realized that babies who go through birth asphyxia may become disabled for life. I found that particularly heart wrenching, especially given that one or two minutes of effective resuscitation could prevent all of that misery.
"…I realized that babies who go through birth asphyxia may become disabled for life. I found that particularly heart wrenching…"
What key insight was most important to guiding the design of your solution?
As a resident, I was trained in the technique of resuscitation. There’s a triple maneuver that you have to do with one hand – head tilt, chin lift, jaw thrust. That same hand also has to perform the E and C clamp technique. That’s where two fingers hold the ventilator mask over the nose and mouth in the shape of a C while the bottom three fingers hold the jaw firmly in the shape of an E so that the oxygen mask fits snuggly without any openings around the edges. That's a lot for someone to achieve with just one hand. The other hand is used to do the bagging, which means squeezing the hand-held device that delivers positive pressure ventilation through the mask.
In some ways, it was an obvious realization that if the second hand was free to help with the technical maneuvers and clamping, then maybe resuscitation would be easier and more effective. When my team and I started to look into it, we found in the literature that was actually the case. In one study, having two hands available was shown to reduce mask leakage by 50%. But this study was done with a second operator taking care of the bagging. It confirmed our assumption, but we had to figure out how we could make this happen with a single operator.
How does your solution work?
NeoBreathe is the world’s first and only pedal-operated resuscitation device. The use of a foot pedal to deliver the positive pressure ventilation to the mask frees the operator’s second hand from the task of bagging so it can now be used for positioning the patient and holding the mask with both hands. This reduces leakage by 50%, as we expected.
With two hands, the grip on the mask becomes much more stable, so pressure and volume become more stable too. And our device includes a reusable manometer that allows the operator to observe pressure levels in real time. Along with our proprietary pressure control technology, this makes the procedure safer for the baby.
Using suction to clear the airway can be another important part of resuscitation. But, depending on where the resuscitation is performed, suction may not always be available. For that reason, we integrated suction into our device so that functional suction will be available no matter what.
With regard to field suitability, the device works without the need for electricity or a source of compressed air. These features further decrease risks and improve operator confidence.
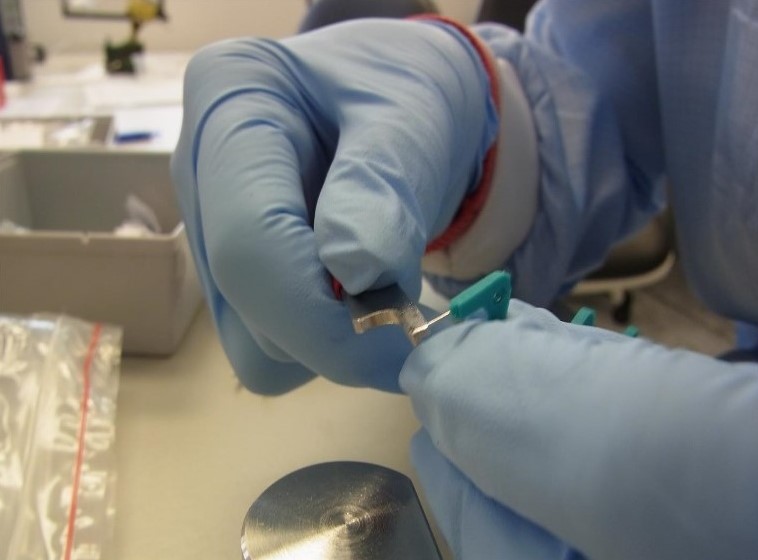
 Avijit Bansal demonstrating the NeoBreathe technology (image credit: Vishal Koul for Outlook Business Magazine).
Avijit Bansal demonstrating the NeoBreathe technology (image credit: Vishal Koul for Outlook Business Magazine).
 This short promotional video, provided by Windmill Health, illustrates how the NeoBreathe technology is intended to work (see endorsement disclaimer below).
This short promotional video, provided by Windmill Health, illustrates how the NeoBreathe technology is intended to work (see endorsement disclaimer below).
At what stage of development is the solution?
NeoBreathe is commercially available in India and 10 other countries, primarily in Africa.
Tell us about a major obstacle you encountered and how you overcame it.
Resuscitation has been done by hand for many decades around the world. Some people find the use of a foot pedal to be a substantial shift. This is particularly true of influential opinion leaders who neither lack skill nor manpower. The way we’ve tried to address this is to create user-friendly, video-based training materials that our distributors can share.
Another big challenge is how slow the government has been to adopt new health technology innovations. The government is the custodian of healthcare in this country for the communities we seek to serve, so the main way we can reach these target groups is to deploy the technology in the public sector healthcare system. This is a challenge for most medical device innovations in the country, not just us. India needs major systemic reform to ensure that medical innovations can be deployed through the public sector health system promptly, transparently, and while ensuring patient safety and well-being.
"In the current environment, medtech innovators have to jump multiple hoops, meet with numerous stakeholders, conduct multiple trials and pilots, and so on."
In the current environment, medtech innovators have to jump multiple hoops, meet with numerous stakeholders, conduct multiple trials and pilots, and so on. Yet the system for procuring innovative products still has not kicked-in to a meaningful extent. This is unfortunate because the government of India has invested heavily in funding medtech innovation. But now that those innovations are ready to serve patients, the government isn’t prepared to deploy them.
What role did your Biodesign training play in enabling you to design, develop, and/or implement this solution?
The need, of course, is the central theme. The Biodesign approach has been particularly helpful in elucidating what is a need, what is not a need, and for whom, before jumping into solutions.
What advice do you have for other innovators about health technology innovation?
Don't just go after needs. Chase demand too. Many times, addressing a need is not enough. The need must be accompanied by demand for a solution. And that demand must be validated with as much painstaking attention as we use to validate the need.
Avijit Bansal co-founded Windmill Health, maker of NeoBreathe, in 2011 out of the Stanford-India Biodesign program.
Disclaimer of Endorsement: All references to specific products, companies, or services, including links to external sites, are for educational purposes only and do not constitute or imply an endorsement by the Byers Center for Biodesign or Stanford University.
Nish Chasmawala and Amit Sharma co-founded Consure Medical out of the 2008 Stanford-India Biodesign program. To learn more, please visit the Consure Medical website.
Disclaimer of Endorsement: All references to specific products, companies, or services, including links to external sites, are for educational purposes only and do not constitute or imply an endorsement by the Byers Center for Biodesign or Stanford University.