Health Technology Showcase
Five Questions and an Elevator Pitch: Serosense
 Members of Team Serosense discuss their solution to help patients suffering from anxiety and depression better adhere to their treatment plans.
Members of Team Serosense discuss their solution to help patients suffering from anxiety and depression better adhere to their treatment plans.
1. What is the need that your project seeks to address?
Suelman: We found that in the treatment of anxiety disorders, there are two major problems – treatments aren’t that efficacious, and they have a significant number of side effects.
Generally, this is how psychiatric treatment currently works: The patient waits a few months to see a doctor. If the diagnosis is anxiety or depression, the doctor prescribes an antidepressant, usually a selective serotonin reuptake inhibitor, or SSRI. It takes four to six weeks for that medication to take effect. And the patient and doctor only know if the drug works, and what the side effect profile is, at the end of that time period.
For a lot of patients, the drug either doesn't work or the side effects are so bad that it doesn't matter if it works. At that point, they start the process again, switching to another medication that also takes four to six weeks to kick in.
A lot of patients will cycle through four or five different medications and then burn out. They might want to drop treatment altogether. This is especially true if they experience gastrointestinal side effects or weight gain. Being able to say, ’Hey, we can avoid the risk of weight gain,’ might be very important for someone who has severe anxiety around body image issues or body dysmorphia.
2. How does your solution work?
Abi: We started out by looking at gastrointestinal side effects because the gut plays a very large role in modulating mental health, mood, and cognition. We wanted to develop a platform that would detect how treatment with SSRIs affects the gut microbiome and what effect this could have on treatment response for mental health disorders such as anxiety and depression.
The way our solution works is we take a skin sample, or a colon sample, and isolate stem cells that we use to grow what are essentially ‘mini guts,’ called colonoids or colon organoids. These are self-growing, self-organizing clusters of cells that represent the gut better than traditional 2D cell cultures.
Ninety percent of the body’s serotonin is produced within the epithelial lining of the gut, so these patient-specific samples have a more physiologically-relevant function and can replicate the native serotonin production in the gut.
We can treat these organoids with SSRIs and measure how serotonin production changes.
Suleman: Long term, we want to be able to say, ‘Based on the types of medications that are used to treat anxiety, these three would give you really brutal side effects so you should avoid them and go with one of these other nine choices instead.’ Or we could say, ’These drugs are most likely to give you the lowest risk of negative side effects.’
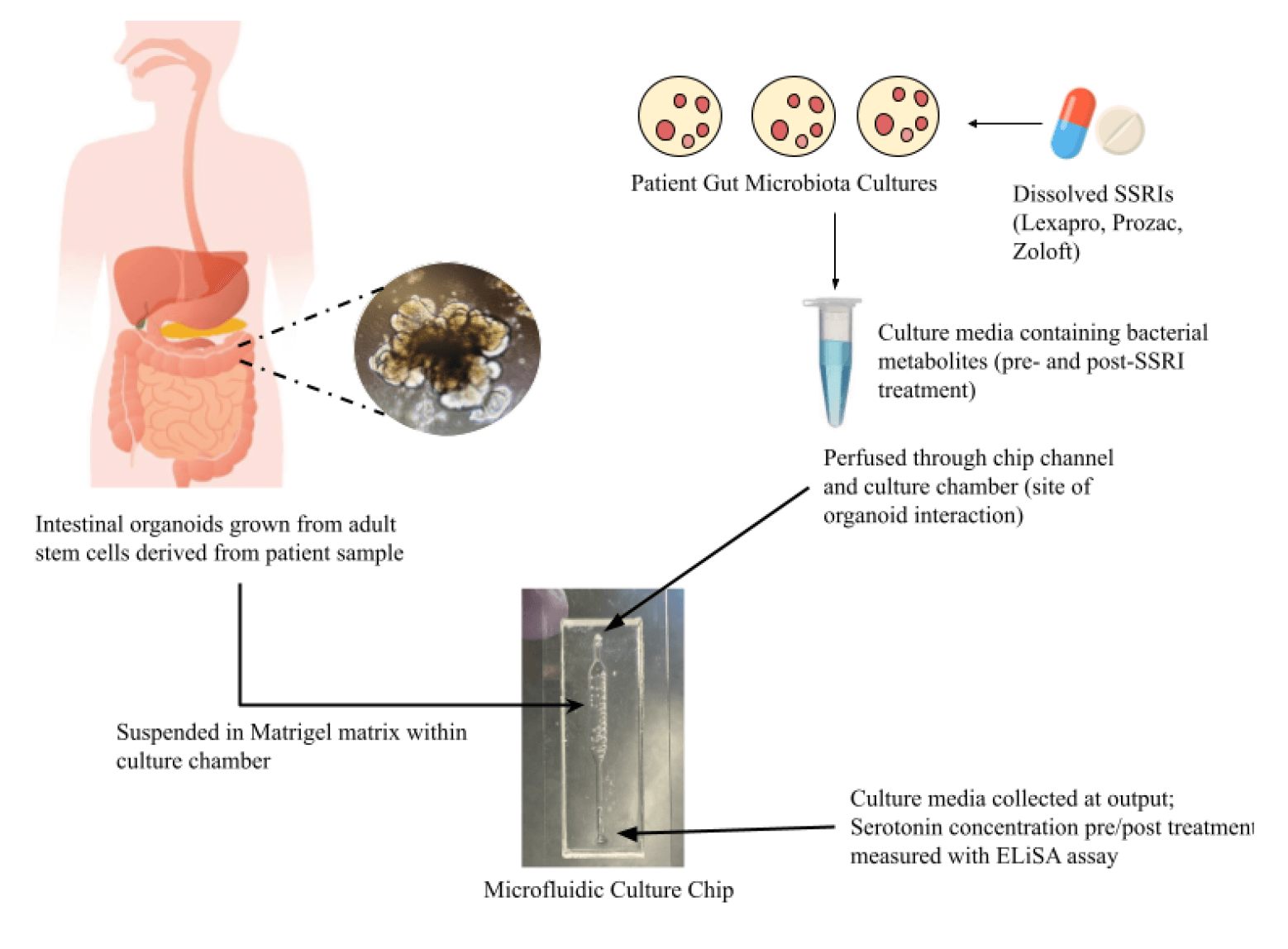 Serosense isolates stem cells from a skin or colon sample and uses them to grow organoids, which can be treated with anti-anxiety drugs to understand likely side effects.
Serosense isolates stem cells from a skin or colon sample and uses them to grow organoids, which can be treated with anti-anxiety drugs to understand likely side effects.
3. What motivated you to take on the project? And what activities have you undertaken?
Abi: Just realizing how activity in the gut can affect the brain was exciting. Being able to map perturbations in the gut to what we're seeing in mental states makes the unknowns of the brain seem more accessible,
Sakina: Last quarter, we worked on a proof of concept model to ensure we're capable of measuring serotonin from our organoids. As a primary experiment, we exposed each of our organoid samples to several common SSRIs. We measured organoid serotonin release over several hours and compared these measurements against organoids without the SSRI treatment.
Suleman: Since then, we have been growing new strands of organoids and redesigning the microfluidic chip that we use. We also talked to Stanford’s Office of Technology Licensing about trying to submit a patent, but we decided to hold off until we develop our project further.
4. What’s the most important thing you learned in advancing your project?
Suleman: You can do a lot more than you think you can if you bug people! And a lot of people are willing to help if you just email them. Progress often takes longer than you anticipate though, because there are so many nitty gritty parts of science that you just can’t hand wave over. You have to pay attention to a lot of very small, sometimes annoying details.
Sakina: I’ll add that sometimes you’ll need help to see a path forward. At one point, we thought our project was impossible and that we needed to change our entire idea. But we are lucky and privileged to have access to mentors and experts who are well-educated in these fields and have relevant real-world experience. For example, we have a mentor from the Kuo Lab who showed us how to mature gut organoids, which would be so much harder if we had to discover that on our own.
5. What advice do you have for other aspiring health technology innovators?
Suleman: I remember several times we wondered, ‘Is this even worth it? Is this idea not feasible? Or dumb? Or has this been done before?’ But it's okay. You will have those existential crises and you will freak out. Just try to stay as calm as you can, and keep yourselves grounded by talking to people who are more experienced than you are.
Abi: Starting with a need we were very passionate about allowed us to stay curious about it. And having an open mind was critical to understanding the real nature of the problem as we went along.
Original team members: Abi Archer, Madeleine Kriz, Emma Lundberg, Suleman Qamar, Sakina Waliji
Course: Bioengineering Capstone
Biodesign NEXT funding: Awarded for spring 2023
