Health Technology Showcase
Five Questions and an Elevator Pitch:
Cerebros
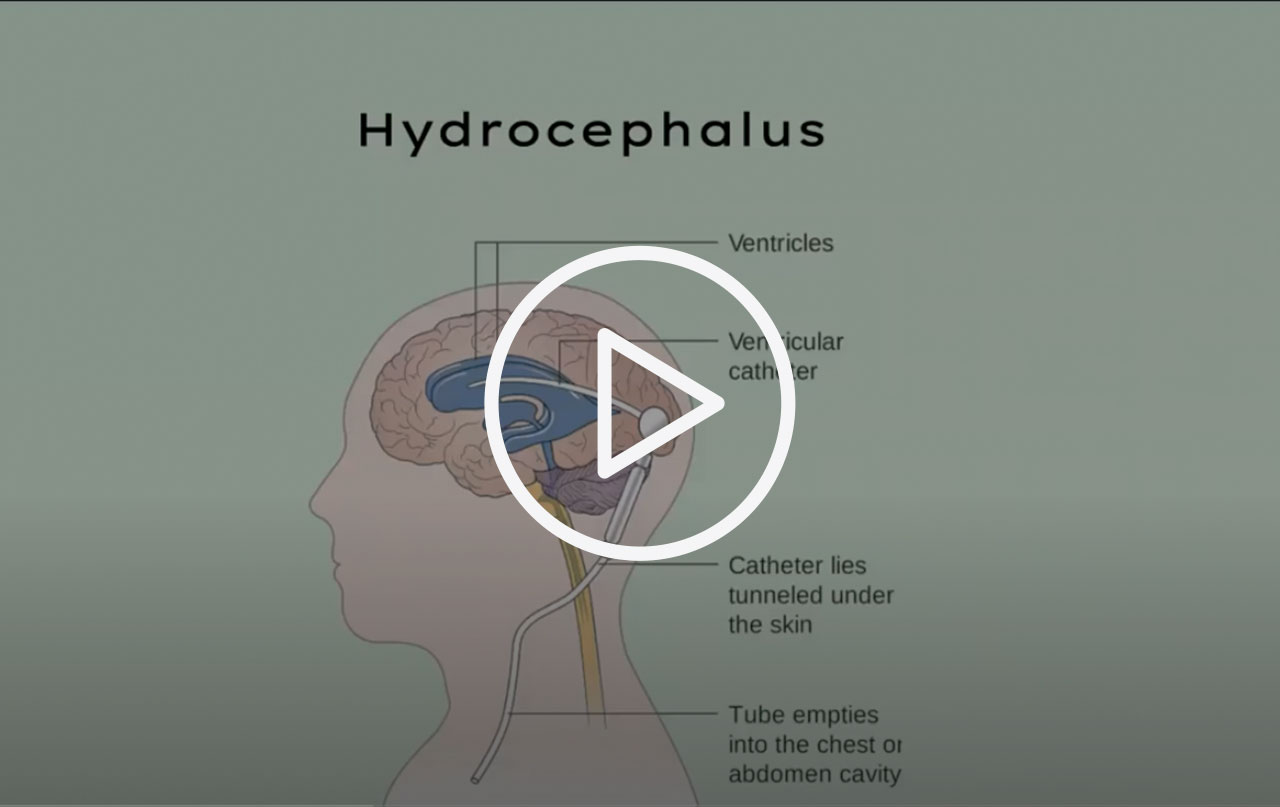 In this short video, members of the Cerebros team explain the need they set out to address and how their solution works.
In this short video, members of the Cerebros team explain the need they set out to address and how their solution works.
1. What is the need your project seeks to address?
Ashlyn: We’re addressing an unmet need in hydrocephalus management. Hydrocephalus is an abnormal build-up of cerebral spinal fluid in the ventricles of the brain. There is no cure; the condition is managed by implanting a shunt to drain the excess fluid into another part of the body. Unfortunately, the shunts are prone to complications. The failure rate within the first two years of implantation can be as high as 50%. After that, blockages or infections can lead to repeated neurosurgical procedures.
One of the biggest problems is that it’s difficult to know when a shunt is failing. The symptoms are vague and nonspecific, often manifesting in the form of headache, nausea, and fatigue. For pediatric patients, especially those who are too young to verbally communicate, these symptoms can be a source of anxiety and guesswork for parents. Obtaining a definitive diagnosis requires a hospital visit and imaging tests that involve exposure to radiation, which is also concerning to parents with young children. So our goal was to find a way to quickly and non-invasively detect shunt failure in order to reduce radiation exposure in hydrocephalus patients.
2. How does your solution work?
Vivek: We believe that in order to improve management, we need to improve measurement. Our solution is a sensor that clips on to the shunt to estimate cerebral spinal fluid flow and alerts the patient and caretaker when there is a shunt failure. It works using a thermal technique that heats a small portion of the shunt, then looks at the temperature profile downstream of the heated region. The information it provides indicates whether or not there is fluid flow occurring within the shunt.
Charles: There are other competing designs that implement the thermodynamics-based detection externally (from the skin surface), but we think an internal device implanted with the shunt is more effective because it bypasses the skin and other tissues surrounding the shunt tube. The major advantage of our internal design compared with the external solution is the reduced heating power requirement, which would be more comfortable for the patient, although it could be harder to replace elements or recharge the battery with an implanted device. The device we’re working on now is meant to be clipped around the shunt tube and implanted at the time of the initial procedure.
3. What motivated you to continue working on your project and what activities did you undertake?
Ashlyn: We wanted to learn more about the patient experience. We had researched the literature to better understand the clinical pathology, but we hadn’t really been able to hear and learn from people living with hydrocephalus. The extension period after class allowed us to dive deep into stakeholder analysis. We connected with patients using Reddit and other social media channels, and then interviewed them to learn about the realities of managing hydrocephalus on a day-to-day basis.
We also used those interviews to incorporate patient voices into our research, design, and prototyping work. We had done some market research, but talking directly with patients helped us assess the value of our solution concept, understand where it fit into the current landscape of hydrocephalus management, and get a better sense for how this technology could be embedded into patients’ everyday lives.
Charles: We also used some of the extension funding to purchase materials and build more realistic prototypes. Because this work occurred when facilities on campus were closed due to COVID-19 restrictions, we weren’t able to access Stanford’s traditional ‘maker spaces’. But we were surprised how much we could accomplish – and learn – doing prototyping at home.
 Early prototype of the Shunt Clip
Early prototype of the Shunt Clip
4. What’s one of the most important things you learned from advancing your project beyond the academic year?
Vivek: This sounds basic, but one of the things we learned was the importance of interacting directly with all the different stakeholders, from patients to doctors. Once you’ve done the clinical research, it’s easy to start assuming things. Those assumptions slowly become accepted by the team as ‘facts’ that influence the decisions that get made. So it’s an essential reality check to interview stakeholders firsthand so you learn if your assumptions could be wrong, and what their actual views on the device and the situation are.
Charles: Similarly, it’s important to stay open-minded and on track from an engineering perspective. As engineers, if we have a hammer, we tend to see everything as a nail. But that’s not good, given that we’re targeting actual applications in patient care, not just solving an engineering question. We learned to keep going back to the users and other stakeholders for feedback as we iterated on the design and development of the device in order to stay focused on what they needed most.
5. What advice do you have for other students who want to become health technology innovators?
Ashlyn: When you’re innovating, you can always make your technology better by asking others to contribute their ideas and inspiration. So I would say be willing to bring in new contributors to help you think in new, creative directions. Innovation is an inherently synergistic, collaborative process, and the more collective and intersectional your knowledge and resources are, the more you can push your ideas.
Original Team Members: Ashlyn Gary, Vivek Gupta, Charles Chen
Course: Biodesign Fundamentals (Med 275 B), spring 2020
Biodesign NEXT Funding: Awarded for summer and fall quarters 2020
