Health Technology Showcase
Five Questions and an Elevator Pitch:
RTHM
 In this short video, two members of the RTHM team explain the need they set out to address and how their solution works.
In this short video, two members of the RTHM team explain the need they set out to address and how their solution works.
1. What it the need your project seeks to address?
Thomas: Rheumatoid arthritis [RA] is a chronic inflammatory disorder in which the immune system attacks healthy joints, resulting in pain, fatigue, swelling, and stiffness. It affects 1.5 million Americans and 22 million people worldwide. RA is one of the costliest chronic diseases because many patients rely on expensive biologic therapies to treat their symptoms. The need we are addressing is a way to make living with rheumatoid arthritis less expensive.
In the typical treatment pathway, when a patient first sees a doctor for RA they receive a prescription for a disease-modifying antirheumatic drug (DMARD) like methotrexate. This is considered a first-line treatment and it can reduce symptoms over time. Three months later, the patient is assessed for improvement. If they are still experiencing moderate to severe symptoms, they are moved to more expensive biologic therapies.
However, a number of studies have been done that showed that first-line medications can be more effective if the medication response is monitored more frequently and the dosage is adjusted in response. The approach is called ‘target to treat,’ and it isn’t done very often because rheumatologists are busy and more frequent monitoring doesn’t fit into their clinical workflow. But when it is used, it’s effective and can bring down overall healthcare costs.
2. How does your solution work?
Thomas: We’re developing a remote monitoring system. Our technology has a wearable component to continuously assesses a patient’s disease activity, combined with a thermal imaging app to capture images of a patient’s hands and provide information about their joints like temperature, swelling, redness, and tenderness. The app also includes a daily survey that patients complete to document their symptoms and how they’re feeling. The combination not only helps patients monitor and manage their own disease activity, but the information is also transmitted to the provider through a software platform. This allows the provider to more easily monitor disease activity and make adjustments to the patient’s medications.
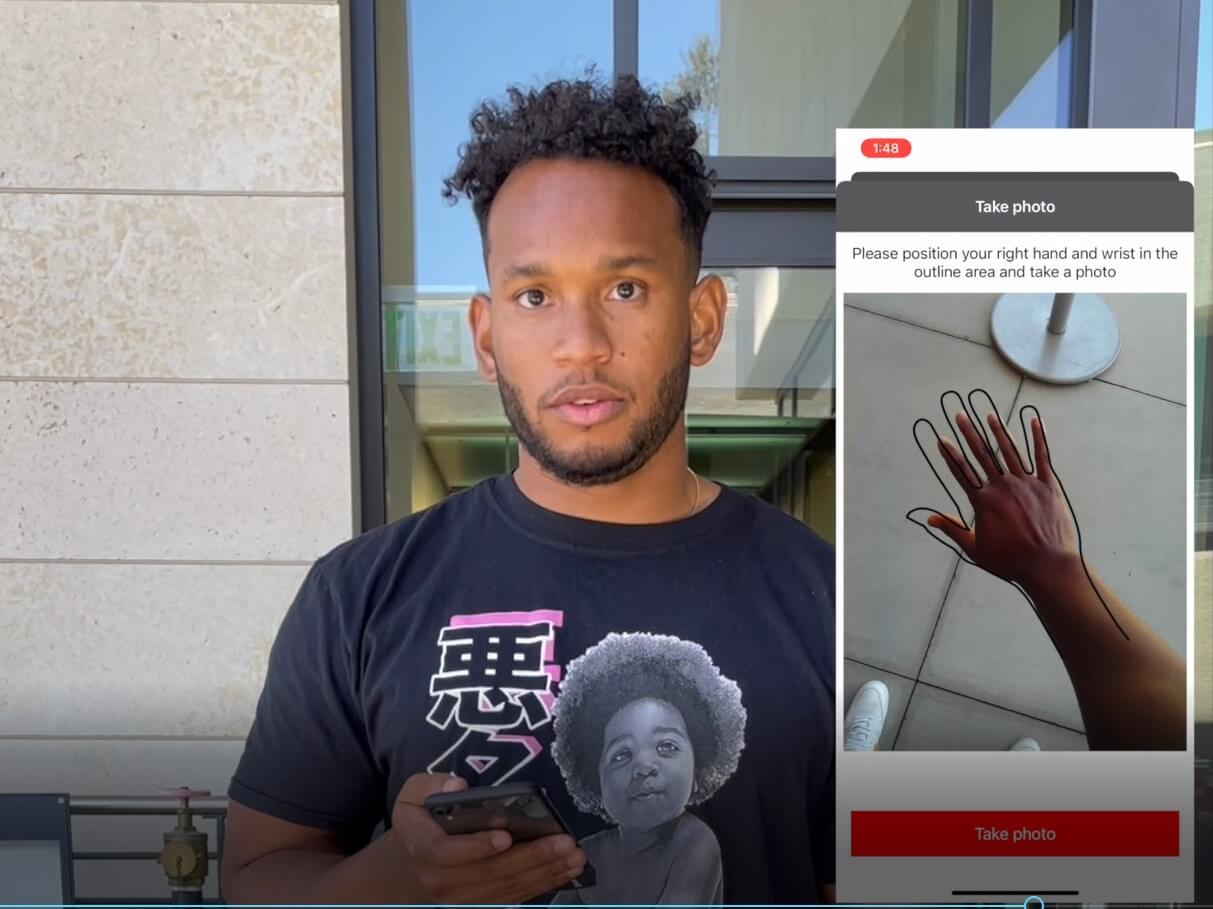 Team member Will Reeves demonstrates RTHM’s hand scan smartphone attachment
Team member Will Reeves demonstrates RTHM’s hand scan smartphone attachment
3. What motivated you to keep working on the project and what activities did you undertake?
Thomas: I was motivated by the idea that I could use my background in immunology to help patients suffering from autoimmune diseases like RA.
With regard to our progress, by the end of the digital health course we had a concept and a design, but we didn’t have an app and we hadn’t developed the wearable. After we got the extension funding, we initiated a research collaboration with Michael Snyder, a genetics professor who is an expert on wearable technology at Stanford. We also worked with an outside software development company to build the thermography component of the application. And we spent more time talking to patients to get a better understanding of the need to help guide our design process. In particular, we used Reddit and subreddits around arthritis to send a survey, and we got back approximately 250 responses that were very helpful.
4. What’s one of the most important things you learned from advancing your project beyond the academic year?
Thomas: One thing I learned was how important it is to go out and talk to the patient population. You can design a technology that is very sophisticated and able to do a lot of fancy things, but if the patient isn’t comfortable using it, or doesn’t enjoy using it to a certain extent, then it’s almost useless.
5. What advice do you have for other students who want to become health technology innovators?
Thomas: Don’t get too attached to the cool technology development part of the process and keep your focus on solving a clinically significant problem.
Original Team Members: Thomas Beck, Bethany Chen, Nick Deveau, Terresa Eun, Keyur Mithawala
Course: Biodesign for Digital Health, fall 2021
Biodesign NEXT Funding: Awarded for winter and spring quarters
